Vaccinations & Immunisations
Shingles Vaccines
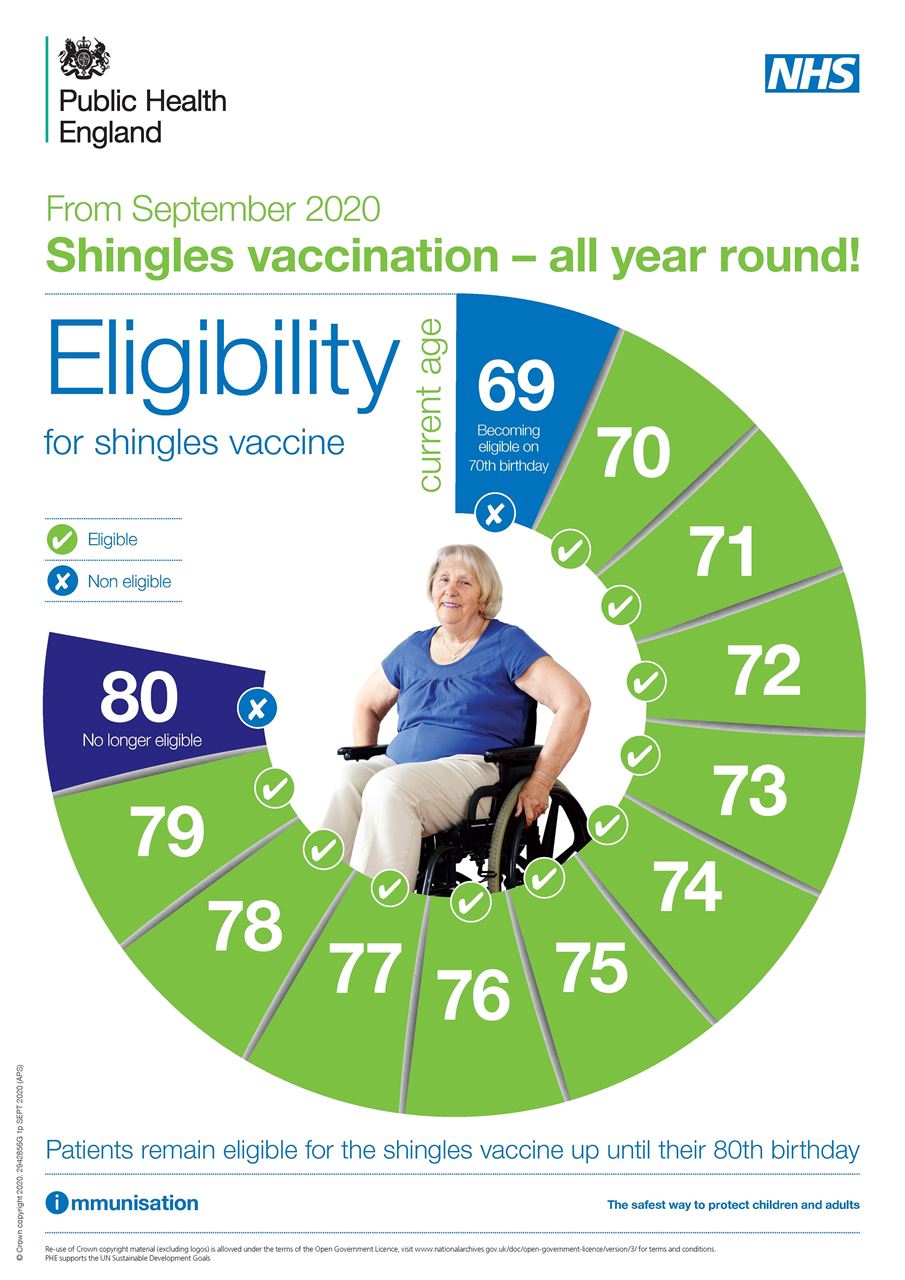
Whitewater Health is committed to delivering this vaccination for its patients including all adults turning 65, those aged 70 to 79 and those aged 50 and over with a severely weakened immune system.. If you are within these guidelines and do not believe you have previously had the shingles vaccine, please do contact us in order for us to administer this for you.
At Whitewater Health we will be making more appointments available for shingles vaccination over the coming months, and will be contacting those who are eligible. Where possible, we can do some vaccinations opportunistically so please do ask your health care professional when you are at the surgery
When you're eligible, you can have the shingles vaccination at any time of year.
The shingles vaccine is not available on the NHS to anyone aged 80 and over because it seems to be less effective in this age group.
Shingles is a common, painful, skin disease. It is caused by the re-activation of the chickenpox virus in people who have already had chickenpox. It begins with a burning sensation in the skin, followed by very painful blisters which turn into sores, before healing. Some people are left with pain lasting years after the initial rash has healed (neuralgia). Shingles is also fatal for around 1 in 1,000 over 70s who develop it.
People tend to get shingles more often as they get older, especially over the age of 70. Unfortunately, the vaccine appears to be less effective in those aged 80 and over.
A vaccine to prevent shingles is available on the NHS to people in their 70s. It is expected to reduce your risk of getting shingles. If you do go on to get shingles, your symptoms may be milder and your illness shorter.
The shingles vaccine can be given at any time of year, and can be given with your annual flu vaccination. It should NOT be given within at least 7 days of a COVID vaccination. The vaccine is likely to offer protection for at least 5 years, probably longer. It is a very safe vaccine and has very few side effects.
As it is a live vaccine, people with a weakened immune system should not have it. This includes individuals on cancer treatment, steroid tablets, immunosuppression treatment (some arthritis treatment for example) and others. Your GP can advise you on this.
More information can be found on the NHS website:
Shingles vaccine overview - NHS (www.nhs.uk)
Pneumococcal Vaccine
The pneumococcal vaccine protects against serious and potentially fatal pneumococcal infections. It's also known as the pneumonia vaccine.
Pneumococcal infections are caused by the bacterium Streptococcus pneumoniae and can lead to pneumonia, septicaemia (a kind of blood poisoning) and meningitis.
At their worst, they can cause permanent brain damage, or even kill.
Who should have the pneumococcal vaccine?
A pneumococcal infection can affect anyone. But some people are at higher risk of serious illness, so it's recommended they're given the pneumococcal vaccination on the NHS.
These include:
- babies
- adults aged 65 or over
- children and adults with certain long-term health conditions, such as a serious heart or kidney condition
How often is the pneumococcal vaccine given?
Babies born on or after 1 January 2020 have 2 doses of pneumococcal vaccine at:
- 12 weeks
- 1 year
Babies born before this date will continue to be offered 3 doses, at 8 and 16 weeks and a booster at 1 year.
Pneumococcal conjugate vaccine (PCV) is used to vaccinate children under 2 years old as part of the NHS vaccination schedule. It's known by the brand name Prevenar 13.
People aged 65 and over only need a single pneumococcal vaccination. This vaccine is not given annually like the flu jab.
Pneumococcal polysaccharide vaccine (PPV) is given to people aged 65 and over and people at high risk because they have long-term health conditions.
People with a long-term health condition may need just a single one-off pneumococcal vaccination or vaccination every 5 years, depending on their underlying health problem.